
I certify that this patient is confined to his/her home and needs intermittent skilled nursing care, physical therapy and/or speech therapy or continues to need occupational therapy. The patient is under my care, and I have authorized services on this plan of care and will periodically review the plan. The patient had a face-to-face encounter with a physician or an allowed non-physician practitioner on 11/01/2020 and the encounter was related to the primary reason for home health care.
Physician or allowed practitioner’s Signature and Date Signed:
Physician or Allowed Practitioner’s Name and Address
John Doe, MD
2121 Washington Pkwy
Suite 220
Washington, DC 20000
NOTE: This represents one example of a valid certification statement. Certification statements can be included in varying forms or formats as long as the content requirements (#1-5 above) for the certification are met.
If the patient is starting home health directly after discharge from an acute/post-acute care setting where the physician or allowed practitioner, with privileges, that cared for the patient in that setting is certifying the patient’s eligibility for the home health benefit, but will not be following the patient after discharge, then the certifying physician or allowed practitioner must identify the community physician or allowed practitioner who will be following the patient after discharge. One of the criteria that must be met for a patient to be considered eligible for the home health benefit is that the patient must be under the care of a physician or allowed practitioner (number 4 listed above). Otherwise, the
certification is not valid.
The certification must be complete prior to when an HHA bills Medicare for reimbursement; however, physicians and allowed practitioners should complete the certification when the plan of care is established, or as soon as possible thereafter. This is longstanding CMS policy as referenced in Pub 100-01, Medicare General Information, Eligibility, and Entitlement Manual, chapter 4, section 30.1. It is not acceptable for HHAs to wait until the end of a 60-day certification period to obtain a completed certification/recertification.
Who can perform a Face to Face Encounter?
Per Medicare Benefit Policy Manual (30.5.1.1) the following can perform a Face to Face Encounter.
When Should a Face to Face Encounter Occur?
The Face to Face encounter "must occur" no more than 90 days prior to the home health start of care date or within 30 days after the start of care. Note: "In situations when a physician or allowed practitioner orders home health care for the patient based on a new condition that was not evident during a visit within the 90 days prior to start of care, the physician or an allowed NPP must see the patient again within 30 days after admission. Specifically, if a patient saw the physician or NPP within the 90 days prior to start of care, another encounter would be needed if the patient’s condition had changed to the extent that standards of practice would indicate that the physician or a non-physician practitioner should examine the patient in order to establish an effective treatment plan." It is best practice to have a face to face with upon admission or intake. Realizing that isn't always possible, the dates are there. Remember, the Face to Face must be signed and dated by the allowed practitioner with the credentials clearly marked. HINT: Don't make auditors look for things. Label documents, highlight them, and make them easy to recognize.
What Should be Included in Face to face documentation?
CMS has said the following items need to be present in the F2F.
Note:
This information can be found most often in clinical and progress notes and discharge summaries. While the face-to-face encounter must be related to the primary reason for home health services, the patient’s skilled need and homebound status can be substantiated through an examination of all submitted medical record documentation from the certifying physician or allowed practitioner, acute/post-acute care facility, and/or HHA (see below). The synthesis of progress notes, diagnostic findings, medications, nursing notes, etc., help to create a longitudinal clinical picture of the patient’s health status.
CGS, one of the CMS Medicare Approved Contractors, has resources for F2F documentation as well. Here's what CGS says. You can find their website here
To be eligible for the home health benefit, a physician must certify that the patient meets the following requirements.
The home health agencies generated medical record documentation, by itself, is not sufficient in demonstrating the patient's eligibility for the home health benefit. Therefore, home health documentation such as, an admit summary, part of the OASIS, or a therapy evaluation/therapy notes, nurses notes that support the certification must be signed off by the certifying physician and incorporated into the physician or acute/post-acute care facility's medical record to help support the FTF. Documentation must correspond to the dates of service being billed and not contradict the certifying physician's and/or the acute/post-acute care facility's own documentation or medical record entries.
Documentation from the certifying physician's medical records and/or the acute /post-acute care facility's medical records (if the patient was directly admitted to home health) used to support the certification of home health eligibility must be provided, upon request, to the home health agency, review entities, and/or the Centers for Medicare and Medicaid Services (CMS).
The certifying physician and/or the acute/post-acute care facility medical record (if the patient was directly admitted to home health) for the patient must contain the actual clinical note for the face-to-face encounter visit that demonstrates that the encounter:
This information can be found most often in clinical and progress notes and discharge summaries.
Conclusion
As seemingly simple as F2F documentation is, agencies continue to struggle with having compliant F2F. The primary diagnosis being related for the primary reason, lack of signature and date (with credentials) and the timeframe are the most common reasons. Our experience, having dealt with a lot of ADRs, is that many MACs and Supplemental Medical Record Contractors (SMRC) interpret the rules inaccurately or incompletely. Denials are often subjective, and sometimes erroneous- often around homebound status and need for services, because the regulations clearly state that these can be demonstrated through the record. Here's a plug for defensible documentation in OASIS. To read that blog called OASIS Documentation for Dummies. We have to document the why so we can demonstrate medical necessity and reasonable and prudent care. Often, auditors are looking for a reason to deny- any reason- even if incorrect.
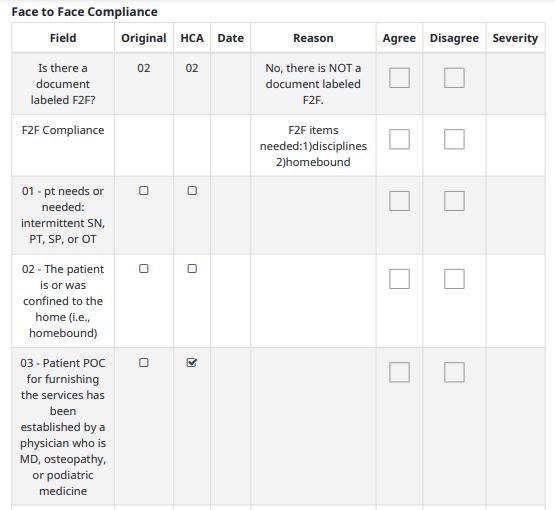
Home Care Answers has prepared many ADRs for agencies. We're happy to help. We're happier to help by ensuring coding and OASIS is correct so that when ADRs come, it's a little less stressful. One of the things Home Care Answers does is share with every chart the face to face compliance. Note- we do not interpret the validity of a F2F because auditors are unpredictable. We share if the items are present in the entirety of the chart. This allows agencies to know what is missing.
Home Care Answers strives to help agencies be compliant. Ultimately, it is on the agency to be compliant, but we try to help. Not only do we strive to provide the most accurate OASIS and Coding to ensure compliance and maximize revenue, we want to provide agencies with the tools to help themselves be successful. We want to create value for agencies.