
What is the Most Common Diagnosis for Home Health Care?
Every agency often asks a similar question. "What's the most common code for home health care?" However, that is somewhat difficult to answer because there are reasons behind that data. Perhaps a major client partner of ours is a major player in a certain referral source in an area and that can have the potential to disproportionately impact the statistics or data showing a trend that may or may not be statistically significant for the entire industry. Naturally, we're a little hesitant to share some of that data and the frequency of the code.
So, in order to show data AND have it supported by outside data, we did some further research. But so has CMS as well. This will be a case study on CMS reliance on data and how agencies can use the data to inform strategy and future plans.
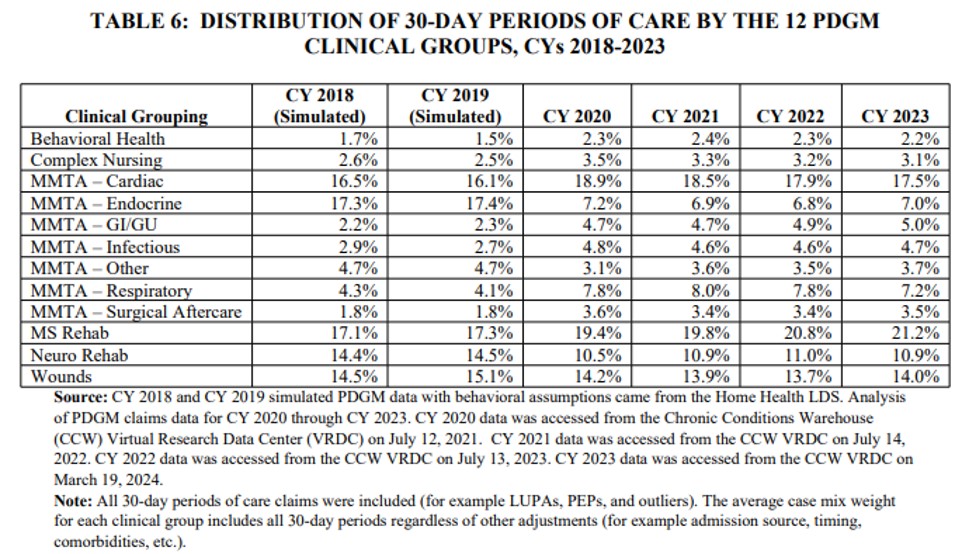
In the 2025 Home Health Proposed Rule, CMS included a table that shows the distribution of the most common clinical groupings over the last several years. The clinical grouping assignment is determined by the primary diagnosis for the visit or the code that goes into the slot on M1021 on the OASIS form. Interestingly enough, MS Rehab is the most common clinical grouping and that is growing as the most common clinical grouping over time. You can see that below.
Z47.1 (Aftercare following joint replacement surgery) is a very common code that is used for all sorts of patients. It's kind of a catch all. That falls into the group MS Rehab under PDGM. If you wonder what the clinical groups are, you can read about it here and you can read about PDGM as well which give the basis for clinical groups. If you want to find out how to read a HIPPS score, which tells you which clinical group any patient is in, you can read that here.
What is interesting is that also in the home health proposed rule, the clinical group of MS Rehab is also proposed to have a 2% reduction in reimbursement. Agencies have focused on ortho patients over time for a long time. Prior to PDGM, agencies could care for orthopedic patients that had joint replacements. Pre-PDGM, agencies would care for a patient for 28 days or so and discharge the patient after they had improved. Agencies would also be paid for a full 60-day episode so long as the patient was not a LUPA patient. Agencies would be paid the full episode for giving half an episode in care. With PDGM, CMS addressed this issue by introducing two 30-day billing periods in the 60 day episode. So, if an agency discharged on day 28, the agency would be paid for 30 days’ worth of work. (again, assuming no LUPA). With the advancement of technology, doctors and agencies are discharging ortho (joint replacement in particular) patients earlier and earlier, which mean less visits, which means less reimbursement. PDGM is tied to estimated cost of care. So as agencies discharge earlier, then of course they'll be reimbursed with less money. Agencies that focus on orthopedic patients primarily have struggled under PDGM rules. They effectively have had to double the census to keep the same revenue volume. Now with further reduction in reimbursement, orthopedic heavy agencies would do well to diversify to other referral sources in addition to the orthopedic care.
You can read about the proposed final rule from CMS here.
What does the primary diagnosis represent in home health?
The primary diagnosis represents a code that describes the primary reason home health care is helping a patient. When a patient is referred by a physician for home health, there is a reason for the referral AND a visit called the Face to Face visit needs to happen and be signed by a qualified professional who will oversee the care plan of that patient. The Face to Face has to be related to the primary diagnosis and focus of care. Coding is funny because there are sometimes coding rules that say a code must be coded first in a sequence, and sometimes the first code in the sequence isn't the primary diagnoses state on the Face to Face. Coding rules require the combination codes to be coded in a certain order. But those cases aren't super common, but still are fairly common. Home Health agencies can sometimes be frustrated by coding rules, but they're the rules. We don't make them up. We do, however, have to follow the rules given to us.
Diagnosis coding, essentially, is simply painting a picture, in medical code form, of the condition of a patient by giving a list of diagnoses that have been documented by a physician, hospital Patient Medical History, or history and physical from discharge from a hospital or outpatient facility. As a note, Home Care Answers, as coders, cannot code based off what a nurse says in a narrative alone. The doctor or qualifying medical professional overseeing the care of the patient is the only person who can diagnose medical conditions to be coded. Home Health has the primary diagnosis or reason for care in the OASIS as M1021. The agency then has 24 slots to fill (if necessary) with pertinent and relevant codes to paint the picture. Further complicating things, there are qualifying comorbid conditions that can be coded that indicate a patient is higher acuity, which means that the agency will likely spend more in the cost of care, which will bring increased reimbursement. These codes interact with each other and it can become very complicated and even confusing. That's why painting the most accurate picture is so important for agencies.
What are qualifying diagnoses in home health?
Simply put, CMS wants to find the underlying condition wherever possible with the highest level of specificity as possible. Prior to PDGM, agencies could use symptom codes as valid primary diagnoses. For several years prior to PDGM implementation, agencies would use "Weakness" as the primary diagnosis (R53.1). We see a face to face from a provider stating the "weakness" is the reason for home health care. Providers haven't had to catch on to PDGM rules as much as agencies. The code for weakness is now a non-compliant diagnosis code. Meaning, the code isn't valid and won't be paid by CMS if submitted for payment. Agencies then must tie the underlying condition which causes the weakness as the primary diagnosis. For example, if a patient is referred to home health for weakness and also has dementia then the agency can code dementia as the underlying cause of the weakness. The agency and provider need to document on the face to face the relationship as the underlying condition. It can be simply patient is referred to home health for weakness due to dementia, which is a perfectly acceptable F2F and primary diagnosis code.
Why does coding matter in home health?
Home Care Answers want to ensure that the correct picture is being painted for CMS so agencies are accurately and fairly reimbursed for the great work they're doing. With only US based coders, we provide top quality work and create value for agencies. Increased accuracy has led to increased reimbursement. But increased accuracy has also led to increased compliance and reduced denials. The primary diagnosis is the start of the claim. Rather than just having a code, it is essential to have the right code. Home Care Answers helps ensure that the right code is used. Find out how we can help for free.